No cell is an island. Our bodies are a complex and continuous series of interactions among trillions of individual living cells. To thrive, cells must process and respond to inputs from surrounding cells, as well as to environmental factors.
Understanding the signals to which a cell responds, and how these responses differ in health and disease, has been an important focus of medical research. The discovery of endocrine and exocrine function, or how cells respond to input from distant cells, has transformed our understanding of pathologies as diverse as diabetes, infertility, and cancer, and how we treat these diseases. The discovery of paracrine function, or how cells respond to input from neighboring cells, has led to new insights and treatments for serious diseases such as Alzheimer’s disease, rheumatoid arthritis, inflammatory bowel disease, and cancer.
Until recently, biologists tended to focus their attention on living cells and their interactions with other living cells. (There’s a reason Lewis Thomas’s 1974 popular science classic was called The Lives of a Cell.) But it turns out that at the scale of our cells, another fundamental, but overlooked, feature of human biology is the interaction of living cells with dying cells.
Generally, life scientists have anthropomorphized the loss of a cell as “cell death.” But the human body is in fact a closely calibrated equilibrium between cell construction and cell disassembly, as billions of cells every day are built through mitosis or retired through myriad distinct mechanisms. When this homeostasis fails and cell disassembly goes awry or begins to outrun cell birth—or the reverse, in the case of cancer—is when trouble starts for the organism as a whole.
Amid these relentless waves of cellular addition and subtraction, which operate as impersonally as a piece of accounting software, scientists are learning that the answer to the question, Did the loss of this particular cell make a difference to tissues? is often yes. That insight may be the start of a new approach to developing medicines that stop disease and keep us in healthy equilibrium longer.
The whole story of cell loss
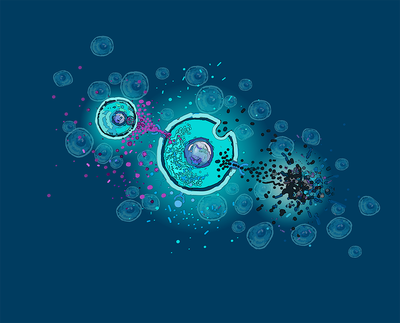
In the 1970s, researchers discovered a tidy, purposeful, and regulated means by which cells disassembled and removed themselves—a kind of altruistic cellular suicide. A genetically programmed cascade of molecular signals can cause a cell to shrink and fragment into tiny blobs that melt into the background without causing inflammation. Biologists realized that this phenomenon, christened apoptosis, was critical to processes like embryogenesis, when temporary structures such as the webbing between fetal fingers or toes must disappear on schedule. And it turned out to be a completely normal aspect of cellular turnover, involved with the removal of billions of cells in our adult bodies each hour. Conversely, pathologic forms of cell loss were called “necrosis” and associated with violent but simple causes: trauma or infection caused dying cells to rupture and empty their contents, sparking inflammation in nearby tissue and attracting white blood cells called macrophages to engulf the debris and clean up the mess.
But that wasn’t the whole story. In recent years, researchers have discovered more and more forms of programmed cell death, each defined by its own chain of gene expression and protein signaling, and each ending in its own way. Dying cells can release a burst of proteins called cytokines that signal infection, or fill up with watery compartments called vacuoles, or see the oxidation of membrane lipid molecules lead the cell to swell and erupt violently into the surrounding milieu.
If a cell, in response to different toxins or diseases, can die in many different ways, do living cells respond in different ways to the material released by cells undergoing different types of cell death? Wouldn’t it make sense that other cells, in their quest to survive, seek to glean information about the sudden loss of their neighbors?
Over the last two decades researchers have been scrambling to identify and label all the myriad ways cells can perish, but they’ve rarely thought to ask how living cells responded, whether the loss of an individual cell influenced these survivors in useful ways, and whether that effect differed depending on the cause of death. Cell-death researchers were acting like forensic investigators who spend all their time documenting a crime scene but forget to give their findings to police and prosecutors.